Doctor Hoo:
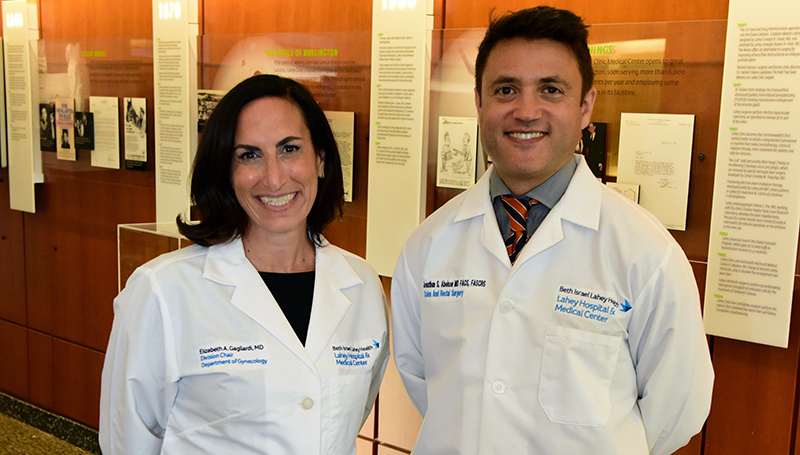
Liz Gagliardi, MD, and Jonathan Abelson, MD
Meet Liz Gagliardi, MD '05, and Jonathan Abelson, MD '12, whose unique partnership is pioneering a multi-disciplinary approach to endometriosis treatment
At Lahey Hospital and Medical Center in Burlington, Mass., a unique partnership is reshaping the way complex endometriosis is treated. Liz Gagliardi, MD ’05, chair of gynecology, and Jonathan Abelson, MD ’12, a colorectal surgeon, are not only colleagues but also University of Virginia School of Medicine alumni whose shared values and complementary skills have led to a collaborative partnership. Together, they are pioneering a multidisciplinary, patient-centered approach that is drawing patients from across New England—and setting a new standard for surgical care.
Parallel Paths to the OR
Though their journeys to medicine were distinct, both Gagliardi and Abelson found their calling in the operating room.
Gagliardi, originally from Melrose, Mass., studied foreign affairs at UVA before pivoting to medicine. After a post-baccalaureate program and a job in admissions at George Washington University, she returned to Charlottesville for medical school in 2001. Initially drawn to pediatrics, she quickly fell in love with OB/GYN during her first rotation. “I loved the thrill of delivering a baby and being in the OR—both things I didn’t think I would enjoy,” she recalls. Her passion solidified around minimally invasive gynecologic surgery, particularly for conditions like endometriosis and fibroids, where she saw a gap in care and a chance to make a difference.
Abelson, who grew up in Scarsdale, New York, studied bioengineering at the University of Pennsylvania and worked in healthcare consulting before deciding to pursue medicine. He entered the UVA School of Medicine in 2008 and eventually decided to pursue a career in surgery because he says it was where he felt most “invigorated.” After completing a general surgery residency at Weill Cornell back in his home state, he chose colorectal surgery as his specialty for its balance of long-term patient relationships and elective procedures. “With colorectal surgery, you can follow patients for years and years. Also, colorectal surgeons are pretty low-key and have a good sense of humor, which I think describes me pretty well,” Abelson says.
A Meeting of Minds and Specialties
When Gagliardi joined Lahey in 2024, Abelson immediately made her feel welcome. “My first day, Jon found me in the hallway and said, ‘Hey, I saw the announcement that you are joining Lahey. I’m so excited to work with you,’” she remembers. Within a week, they were planning their first joint surgery.
Their collaboration quickly became something rare: a gynecologist and a colorectal surgeon operating together multiple times a week. “We have a huge, complex endometriosis population coming from all over New England,” Gagliardi explains. “Many endometriosis patients wish to maintain their fertility, so it’s not so easy for us to just say, ‘We’re going to come in and take out your colon and take out your uterus, and that will make things better.’ It’s really an art form. Some patients want us just to return their anatomy to their normal locations. Some of them want us to excise all of their disease, so we truly cater our practice to each individual patient.”
Their teamwork is built on constant communication and mutual respect. Both are trained in robotic surgery, often sitting side-by-side at consoles during procedures. “We spend a lot of time not just doing endometriosis but also treating patients who have colorectal cancer that involves their GYN organs as well. It has become a symbiotic relationship where we help each other a lot in the OR,” Gagliardi says.
Their collaboration extends beyond gynecological and colorectal patients. They also work closely with urology and thoracic colleagues. The synergy is so strong that Lahey is giving them a dedicated joint OR block in recognition of their integrated model.
Robotics and the Future of Surgery
Central to their work is the DaVinci DV5 robotic platform. They were the first surgeons in New England to acquire the technology, which includes a new feature called telepresence.
“Telepresence means I can call another robotic surgeon anywhere in our network and say, ‘Hey, I need a consult. Can you look at this?’” Gagliardi explains. “We actually did the first telepresence case in the United States. Jon was in his office, and I was in the OR. He was able to see what I was doing live during the surgery and talk to me through the speakers.”
The implications are profound. Gagliardi, who precepts surgeons nationwide, sees telepresence as a way to support providers in underserved areas who don’t have mentors—helping them improve their skills and better serve their communities.
While there isn’t a lot of clinical data yet to show that robotic surgery is superior to other approaches, Abelson believes it represents the future. He and Gagliardi both cite enhanced imaging and greater surgical precision as key benefits, along with ergonomic advantages. “We’re not hunched over at the bedside anymore. We’re sitting at a console, which helps with surgeon longevity,” he says.
For most surgeons, the decision to use robotics ultimately comes down to comfort and training. “The general approach is you try to do minimally invasive when possible, and then whatever instrument or tool is your preferred approach—that’s what you want your surgeon to use,” he says.
What’s Next?
Their success in the OR has inspired a broader vision: establishing a multidisciplinary Endometriosis Center of Excellence at Lahey. The hospital already holds the designation for Minimally Invasive Gynecologic Surgery, but Gagliardi and Abelson are hoping for recognition of their unique, team-based approach and have submitted paperwork for the new accreditation.
In the meantime, they have launched a multidisciplinary endometriosis conference that includes urology, thoracic surgery, pathology, and radiology. Cases involving three or more services are presented, and discussions have included topics like conservative vs. radical surgical approaches and the complications that come with preserving fertility. “It’s created a lot of good conversation and a lot of good ideas for research as well across all of our divisions,” Gagliardi says. “It’s the first time I’ve really seen it done for a benign disease, where the patients truly get all of the experts in a room reviewing their case pre-op and post-op. I love the thought that we’re doing something innovative in that area.”
Abelson says that sharing what they’ve learned by providing on-site mentoring opportunities is also a goal. “We would love to host surgeons—from the GYN surgeon, the colorectal surgeon, the urology surgeon, the thoracic surgeon—and basically line up a couple of cases in a day. They could come the day before and we’d have meetings, and they’d come to one of the multidisciplinary conferences, as well as be present in the OR with us to see how we’re deciding which approach to take and how to make those decisions.”
The UVA Thread
Though they didn’t overlap at UVA, both Gagliardi and Abelson credit their medical school experience with shaping their approach to medicine and to each other.
“Medical school was probably one of the best times in my life,” Gagliardi says. “That’s probably a rare thing for people to say, but the friendships I built, the support system—they’re a team that will stay with me forever. When Jon and I started operating together, I realized we had a similar approach in the OR. We value every team member and encourage everyone to share their thoughts and opinions to improve our safety and outcomes. We think everyone has something to add. I think, at least in my opinion, that comes from being at UVA. That was something that I feel like was fostered there, and I think that’s one of the big things I came away with—other than my amazing group of friends.”
Abelson echoes the sentiment. “It was also the best four-year period of my life in some ways. I think Lahey is similar to UVA in that it fosters collaboration and collegiality and the idea that every single person is ultimately here to help patients,” he says. “I think the fact that we were able to experience that at UVA, and now we’ve been able to find that here at Lahey is incredible. It’s a really great opportunity. I feel very fortunate to be able to participate in that culture.”


